In line with most fields of medicine, litigation involving oral and maxillofacial surgery (OMFS) is increasing, as is the amount paid out in compensation (1), although OMFS claims result, on average, in the lowest amount paid per claim of all the surgical specialities (2). According to the NHS Litigation Authority, between 1995 and 2010 a total of 318 claims relating to OMFS were registered with them and a total of £5 million in compensation was paid out (1). Mr Zaid Sadiq, Consultant Oral and Maxillofacial Surgeon discusses the challenges of assessing patients with dental, cranial or facial conditions.
While most claims relate to dentoalveolar surgery and minor oral surgery, such as third molar extractions, this is not entirely surprising considering the high volume of patients treated (1,3,4). The most common complications of this type of surgery are lingual nerve damage, postoperative infection, wrong site extractions and in rare cases death (3–6). Many factors influence the incidence of complications after third molar extraction and these include age, medical history, poor oral hygiene, smoking status, type of impaction, surgical and/or anaesthetic technique used and the experience of the surgeon (6). Therefore, all these factors need to be taken into account when assessing the suitability of the patient for surgery. Other procedures commonly cited in litigation include dental implant surgery, rhinoplasty and orthognathic surgery to correct dentofacial discrepancies, with most complaints centring around infection, implant failure and poor aesthetic results (4,7).
Traumatic injuries to the face and mouth area can cause pain, functional impairment and aesthetic issues and lead to physical, emotional and social consequences both for the patient and for their family. Therefore, when presented with such an injury, a physician should aim to limit the consequences by undertaking a thorough clinical assessment, from which correct treatment can then be planned. Careful initial assessment is paramount, as for some injuries the prognosis is very dependent on early diagnosis and correct management. This is particularly true of dental and facial fractures, as well as tooth avulsions. The main goals of treatment are to avoid or limit complications, and to restore function and aesthetic appearance. Furthermore, physicians must take into account the psychological distress caused to the patient by injuries to the facial area and the ensuing anxiety which follows, as this may have some influence on treatment (8).
It can clearly be seen that in traumatic orofacial injuries, the initial physical examination is extremely important. As well as the examination of clinical signs resulting from obvious trauma, such as bruising , facial bony and soft tissue structures must also be evaluated. The victims of such injuries must also be examined for any signs of head injury which could affect brain and spine function.This should include an assessment of the occlusion, as these could be the result of problems with the temporomandibular joint (TMJ), such as fractures, effusion and/or bleeding into the joint space (8). Issues with the TMJ are a frequent finding in cases of facial trauma but they can be difficult to diagnose as the symptoms are heterogeneous, often multifactorial in origin and can fluctuate over time (9). However, missed TMJ fractures are problematic for the patient, particularly in younger patients as they may result in abnormal or asymmetric facial growth and a reduction in the size of the lower jaw (8) and the number of claims relating to TMJ damage is rising (9) And may predispose to arthritis of the jaw joint in the long run. For this reason, radiological examination should always be performed. Furthermore, intraoral radiography will expose root fractures and tooth displacement or avulsion, while radiography of the soft tissues may identify foreign bodies that are present in wounds. Prompt detection and removal of tooth or bone fragments can be crucial in reducing the risk of subsequent infection (8).
Dental and facial trauma occurs frequently in children and adolescents and the prevalence of this type of injury has risen over recent years. This is due to the increased involvement of children and adolescents in play activities and competitive sports, more widespread usage of motorised vehicles by teenage children and an increase in the number of families keeping pets at home, especially dogs. However, the treatment of dental and facial injuries in children and adolescents presents some additional challenges. Any failure to provide adequate treatment may result in functional deficits and aesthetic issues which can have long-term effects in patients who are still growing. Assessing these injuries can be more difficult though, particularly in very young children who may not be able to describe their symptoms very well (8).
Another issue to consider is the possibility of non-accidental injury, such as child abuse or self-inflicted injury (8). It has been estimated that up to 50% of all the physical injuries associated with child abuse occur in the head and neck area (10). A study of cranio-maxillofacial trauma in children showed that, overall, around 4% of cases were due to violence (11), while it has been reported elsewhere that nearly 20% of injuries to the TMJ are non-accidental (12). TMJ fractures relating to acts of violence are often located in a different area to those resulting from road traffic accidents, so an injury in this area should always raise the possibility of a non-accidental origin. Any injury which leads a clinician to suspect child abuse must always be followed up, as there is a legal obligation to report such abuse. Typical signs might include bruising and abrasions which do not correspond to bony prominences, those which have been caused by recognisable objects such as bites or burning by cigarettes, and lesions which are clearly of different ages and therefore must have occurred at different times. Any discrepancy between the trauma history provided by the parent and the injuries found on examination, differences in the story given by each parent or a delay in presentation should also arouse suspicion (8).
While claims relating to cancers of the head and neck (HNC) are relatively rare (13), the amounts awarded in compensation can be substantial (1). This is due to the cost of care, the potential for pain and disfigurement and the negative impact of the disease on quality of life (14). The most common complaint is of missed or delayed diagnosis (13,14). The epidemiology of HNC and oral cancer among younger patients is changing, due to certain forms of the human papilloma virus and immunosuppression, and the presentation and risk profile of the disease have altered (14). Often, patients are younger than would have been seen previously and therefore a clinician’s expectation that a younger patient has developed the disease may be lower than if presented with an older patient (13,14).
Furthermore, HNC may be difficult to diagnose, as in the early stages the tumours are associated with no or few minor nonspecific symptoms, which may be overlooked by both the patient and health professionals. Mucosal lesions may mimic benign conditions and even advanced-stage cancers can have minimal signs. It is important to remember then that a delay in diagnosis, or even misdiagnosis, may not necessarily reflect a breach of the standard of care given by the doctor or dentist. Diagnosis of the condition requires accurate testing and interpretation of the results. Despite this, it has been reported that in approximately half of HNC cases which resulted in litigation, it was alleged that a biopsy was indicated but not performed (14). A delay in diagnosis may lead to progression of the disease and a poorer outcome, which in turn may increase the likelihood of litigation for alleged malpractice. However, outcome is also closely linked to the biology of the tumour, so a poor result does not necessarily indicate negligence by the healthcare team (13,14).
While every surgical procedure carries a risk of complications, OMFS may be particularly prone to claims of negligence due to the aesthetic implications of many of the procedures carried out. Fortunately, serious complications are relatively rare and although claims for minor complications are fairly common, the level of compensation awarded per incident is comparatively low. However, this should not stop an OMFS specialist from carrying out a thorough assessment of each patient and providing a full explanation of the potential risks of the procedure to be carried out. In cosmetic procedures, the patient should be given realistic expectations of the likely aesthetic outcome. For any procedure, the patient should, if necessary, be referred to a more experienced or specialist dentist or doctor, in order to minimise the risk of a claim occurring (14).
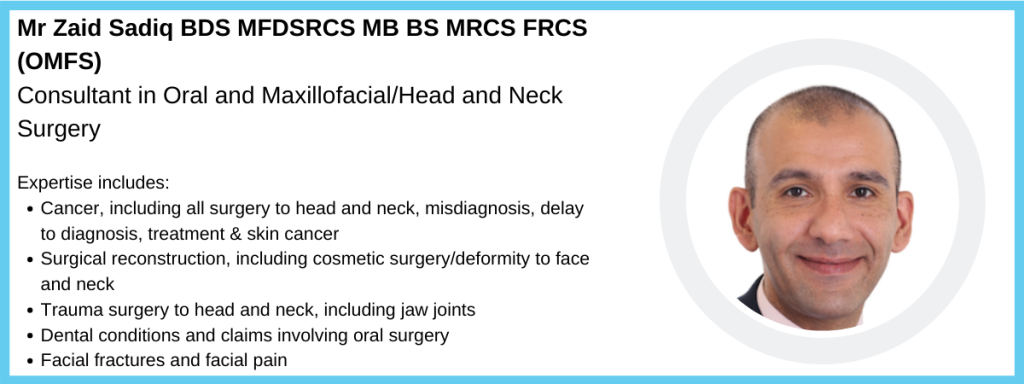
About Mr Zaid Sadiq, Consultant Oral and Maxillofacial Surgeon
Mr Zaid Sadiq, is a Consultant Oral and Maxillofacial/Head and Neck Surgeon at the Queen Victoria Hospital prior to which he worked for many years at other leading hospitals including University College London Hospital and Great Ormond Street.
Mr Sadiq is qualified in both medicine and dentistry. He completed higher surgical training in Oral and Maxillofacial Surgery in the London KSS region. He completed a Head and Neck reconstruction fellowship in Edinburgh and is accredited by the Royal College of Surgeons of England. He is an honorary lecturer at University College London.
Mr Sadiq has a keen interest in cancer, reconstructive surgery and tissue engineering, as well as providing a spectrum of oral and maxillofacial practice.
References
- Gulati A, Herd MK, Nimako M, Anand R, Brennan PA. Litigation in National Health Service oral and maxillofacial surgery: review of thelast 15 years. Br J Oral Maxillofac Surg. 2012 Jul;50(5):385–8.
- Ford KE, Cooper LRL. Learning from lawsuits: Ten-years of NHS litigation authority claims against 11surgical specialities in England. Surgeon. 2018 Feb;16(1):27–35.
- Boffano P, Roccia F, Gallesio C. Lingual nerve deficit following mandibular third molar removal: review of theliterature and medicolegal considerations. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012 Mar;113(3):e10-8.
- Bordonaba-Leiva S, Gómez-Durán EL, Balibrea JM, Benet-Travé J, Martin-Fumadó C, Bescos Atin C, et al. Twenty four years of oral and maxillofacial surgery malpractice claims in Spain:patient safety lessons to learn. Oral Maxillofac Surg. 2019 Jun;23(2):187–92.
- He P, Mah-Ginn K, Karhade DS, Donoff B, Adeeb N, Gupta R, et al. How Often Do Oral Maxillofacial Surgeons Lose Malpractice Cases and Why? J oral Maxillofac SurgOff J Am Assoc Oral Maxillofac Surg. 2019 Dec;77(12):2422–30.
- Bouloux GF, Steed MB, Perciaccante VJ. Complications of third molar surgery. Oral Maxillofac Surg Clin North Am. 2007 Feb;19(1):117–28, vii.
- Friscia M, Sbordone C, Petrocelli M, Vaira LA, Attanasi F, Cassandro FM, et al. Complications after orthognathic surgery: our experience on 423 cases. Oral Maxillofac Surg. 2017 Jun;21(2):171–7.
- Cagetti MG, Marcoli PA, Berengo M, Cascone P, Cordone L, Defabianis P, et al. Italian guidelines for the prevention and management of dental trauma in children. Ital J Pediatr. 2019 Dec;45(1):157.
- Manfredini D, Bucci MB, Montagna F, Guarda-Nardini L. Temporomandibular disorders assessment: medicolegal considerations in theevidence-based era. J Oral Rehabil. 2011 Feb;38(2):101–19.
- Costello BJ, Papadopoulos H, Ruiz R. Pediatric Craniomaxillofacial Trauma. Clin Pediatr Emerg Med. 2005;6(1):32–40.
- Gassner R, Tuli T, Hächl O, Moreira R, Ulmer H. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuriesin 10 years. J oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2004 Apr;62(4):399–407.
- Monnazzi MS, Gabrielli MAC, Gabrielli MFR, Trivellato AE. Treatment of mandibular condyle fractures. A 20-year review. Dent TraumatolOff Publ Int Assoc Dent Traumatol. 2017 Jun;33(3):175–80.
- Lydiatt DD. Medical malpractice and head and neck cancer. Curr Opin Otolaryngol Head Neck Surg. 2004 Apr;12(2):71–5.
- Epstein JB, Kish R V, Hallajian L, Sciubba J. Head and neck, oral, and oropharyngeal cancer: a review of medicolegal cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015 Feb;119(2):177–86.
